Autoimmune Inner Ear Disease AIED Symptoms and Treatment
Autoimmune inner ear disease is a rare illness in which the immune system accidentally attacks the inner ear.
It can cause dizziness, ringing in the ears, and hearing loss. AIED affects less than 1% of the 28 million Americans who have hearing loss. It is substantially more prevalent in middle-aged women and women in their forties and fifties. Symptoms Hearing loss begins in one ear and progresses to the other in AIED.
This can take weeks or months. Additionally, dizziness and balance problems are indicators and symptoms. Tinnitus (a ringing, hissing, or buzzing sound in the ear) and dizziness (a sensation of spinning) constantly alert your immune cells to the presence of germs seeking to penetrate your body. They misinterpret cells in your inner ear for viruses or germs and attack them. This type of reaction is referred to as an autoimmune response. Immune cells can also cause damage to other organs.
Over 30% of people with AIED have rheumatoid arthritis, lupus, scleroderma, ulcerative colitis, or Sjogren’s syndrome (dry eye syndrome). Because the symptoms of AIED are so prevalent, diagnosing it can be challenging.
It is usually misdiagnosed as an ear infection until the hearing loss has progressed to the second ear. To diagnose AIED, doctors will conduct a physical examination and conduct a hearing test. Additionally, they will do a balance test to see how well your inner ear “communicates” with your brain. Additionally, a blood test is possible. While no test can confirm whether you have AIED, the results may indicate an autoimmune reaction.
If this is the case, you should seek therapy from an ear, nose, and throat specialist familiar with autoimmune diseases. Due to the possibility that you will not acquire a conclusive diagnosis, your doctor may begin therapy without a formal diagnosis to avoid irreparable hearing loss. Many individuals are not diagnosed with AIED until their symptoms improve the following treatment.
Balance Disorders Causes Types Treatment NIDCD
What does it mean to have a balancing issue? A balance problem is a condition that makes you feel unstable or dizzy. Whether you stand, sit, or lie down, you can experience a sense of movement, spinning, or floating. When walking, you may feel as though you’re going to fall over. While everyone experiences dizziness at times, the term “dizziness” can refer to various distinct conditions. Dizziness can range from a transient fainting sensation to a severe episode of vertigo that lasts for an extended time.
Around 15% of individuals in the United States (33 million) reported having a balance or dizziness problem in 2008. Balance problems can be caused by various medical conditions, medications, or a problem with the inner ear or brain. A balance deficit can make everyday tasks more difficult and might result in mental and emotional complications. How can you determine whether you have a balance issue? If you have a balance problem, you may notice the following indications and symptoms.
Headache or dizziness (a feeling of spinning). It was collapsing or anticipated collapsing. It’s a stumbling obstacle when you’re attempting to walk. Feeling lightheaded, faint, or floaty, vision becomes hazy. When someone says bewilderment or disorientation, two things spring to mind: confusion and disorientation. Among the possible symptoms are nausea and vomiting, diarrhoea, changes in heart rate and blood pressure, and dread, concern, or panic. Symptoms may arise and dissipate rapidly or may last for an extended time, resulting in tiredness and despair.
What causes balance disorders?
Balance difficulties can be caused by medication, ear infections, head traumas, and other factors affecting the inner ear or brain. You may suffer dizziness if you stand up too quickly with low blood pressure. Disorders such as arthritis or an imbalance in the eye muscles can also create balance problems in the skeletal or visual systems. The chance of developing balance problems increases with age. Unfortunately, many balance difficulties occur suddenly and without apparent cause.
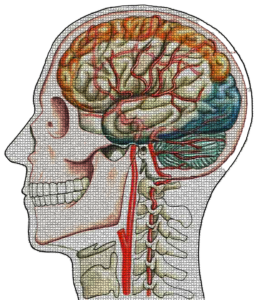
How does my body keep its balance?
Balance is determined by a series of impulses provided to the brain by various organs and structures in the body, most notably the eyes, ears, muscles, and touch receptors in the legs. The vestibular system often referred to as the labyrinth, is a labyrinth-like arrangement of bone and soft tissue in the inner ear that regulates balance and movement. NIH/NIDCD (National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases) vestibular system components of the inner ear The arcuate ducts are present throughout the labyrinth. Three fluid-filled channels create loops within the arcuate ducts, which are virtually perpendicular to one another. When the head rotates, a signal is sent to the brain. Each canal has a cupula [KEW-pyew-lah], a gelatinous substance that spreads like a thick sail and seals off one end.
On top of the cupula is a cluster of sensory hair cells. Stereocilia are tiny, thin extensions from each hair cell into the cupula. When you swivel your head, the fluid in the arcuate moves, making the cupulae flex or undulate like sails in the wind, bending the stereocilia. This bending transmits a nerve signal to the brain, alerting it of the twisting orientation of the head. There are two otoliths [oh-toe-LITH-ic]: the iriticle [YOU-trih-cull] and the saccule [SACK-kewl]. Between the semicircular canals and the semicircular canals is where the cochlea is located (a snail-shaped, fluid-filled structure in the inner ear).
These organs transmit to the brain information about your head’s position concerning gravity, such as whether you’re sitting, reclining, or lying down, as well as any movements your head makes, such as side to side, up or down, forward or backward. The utricle and saccule’s floor and wall are lined with sensory hair cells, with stereocilia extending into a gel-like layer above. Otoconia [oh-toe-CONE-ee-ah] is a term that refers to tiny, thick calcium carbonate grains that are present in this gel. Gravity presses on these grains regardless of the position of your head, causing the stereocilia to change, signalling the status of your brain. Each movement of your head transmits a signal to your brain, alerting it of the change in location of your head.
When you move, your vestibular system detects mechanical forces such as gravity and stimulates the arcuate and auricular organs. Other sensory systems in your body, such as vision and the musculoskeletal sensory system, collaborate with these organs to regulate your body’s posture at rest or inaction. This assists you in maintaining a firm stance and balance when you walk or run. Additionally, it aids you in keeping visual attention on items when your body is in motion. If any of these sensory system signals are disrupted, you may have balance difficulties, such as dizziness or vertigo.
Additionally, if you have issues with motor control, such as weakness, slowing down, tremors, or stiffness, you may lose your ability to recover from an imbalance properly. As a result, falls and injuries are more probable. What are the many types of balance disorders? Balance problems manifest themselves in several ways. The following are just a handful of the more common.
BPPV, sometimes referred to as positional vertigo, is a brief, acute episode of dizziness caused by a particular change in head position. It is a form of benign paroxysmal positional vertigo. When you bend down to inspect something beneath your feet, tilt your head to look up or over your shoulder or turn over in bed, you may have a sense of spinning. BPPV is caused by loose otoconia entering one of the arcuate channels and impairing the function of the cupula. This damages the cupula’s ability to flex correctly, resulting in vertigo by delivering incorrect information to the brain regarding the head’s location. BPPV can occur as a result of a concussion or as a natural part of ageing.
Dizziness and balance problems are caused by labyrinthitis, an infection or inflammation of the inner ear. It typically occurs in conjunction with an upper respiratory illness, such as influenza. Ménière’s disease is characterised by dizziness, hearing loss, tinnitus (a ringing or buzzing in the ear), and a sensation of fullness in the ear. It may be related to a change in fluid in certain parts of the labyrinth; however, the cause(s) is unclear. Ménière’s disease is explained in-depth on the National Institute of Diabetes and Digestive and Kidney Diseases’ web page Ménière’s disease.
Vestibular neuronitis: Inflammation of the vestibular nerve caused by a virus that often manifests as vertigo.
Perilymph fistula:
Middle ear fluid is seeping from the inner ear. It causes agitation, nausea, and dizziness, which usually increases with exercise. A perilymph fistula can occur due to a head injury, significant changes in air pressure (e.g., scuba diving), physical exertion, ear surgery, or chronic ear infections. A perilymph fistula is a congenital disability. MdDS (Mal de Debarquement Syndrome) is a continuous rocking, swaying, or rocking sensation during a cruise or other nautical adventure or even after prolonged treadmill jogging. Symptoms often subside within hours or days of landing or quitting to use the treadmill.
On the other hand, severe instances may persist for months or even years for unexplained reasons. What procedures are used to determine whether or not an individual has a balance disorder? A balance problem is notoriously difficult to identify. Your primary care physician may send you to an otolaryngologist and an audiologist to evaluate if you have a balance problem. Otolaryngologists are physicians and surgeons who specialise in illnesses and disorders of the ears, nose, throat, and pharynx. An audiologist is a professional who specialises in the function of the auditory and vestibular systems. The Epley manoeuvre is used to remove otoconia. You may be subjected to hearing tests, blood tests, a videonystagmogram (a test that analyses eye movements and the muscles that control them), or imaging scans of your head and brain.
Another potential test is posturography. You will be positioned in front of a patterned screen on a customised moving platform for this exam. Posturography is a balancing test that assesses your ability to keep your balance in various settings, including standing on a stationary moving surface. Additional examinations, such as swivel chair tests, severe headshake tests, or tests evaluating the eye or neck muscles’ reaction to harsh clicking noises, may be performed. Due to the complexity of the vestibular system, several tests may be necessary to determine the root of your balance problem.
How are balance disorders treated?
An ENT expert will first determine whether another disease or medication is causing your balance problems. Your doctor will either treat the issue directly, prescribe a different medicine, or refer you to a specialist if the illness falls outside of their scope of practice. If you are diagnosed with BPPV, your otolaryngologist or audiologist may conduct a series of minor procedures, such as the Epley technique, to dislodge the otoconia from the archway. While a single session is frequently sufficient, the therapy must be repeated multiple times until vertigo subsides for other individuals.
If you are diagnosed with Ménière’s disease, your ENT specialist may urge you to make dietary changes and quit if you are a smoker. While medicines for dizziness and nausea may help you feel better, they may also make you drowsy. Other medications, such as gentamicin (an antibiotic) or corticosteroids, may be used. While gentamicin is more effective than corticosteroids at reducing dizziness, it might cause permanent hearing loss in some people.
In some severe cases of Ménière’s disease, the vestibular organs may require surgery. Specific individuals with vestibular problems are unable to eradicate their dizziness and must learn to cope. A vestibular rehabilitation therapist can aid you in developing a personalised therapy plan. Consult your physician to determine whether driving is safe for you and how to minimise your risk of falls and injuries while performing routine tasks such as walking up or downstairs, going to the bathroom, or exercising. Avoid walking in the dark to minimise the risk of injury caused by dizziness. Wear low-heeled or walking shoes when walking outside.
If necessary, utilise a cane or walker. And make modifications to your home and work environment, such as installing railings. When should I seek assistance if I believe I am having difficulty maintaining my balance? Ask yourself the following questions to ascertain if you should consult a physician for dizziness or balance concerns. If you answered “yes” to any of the following questions, you should consult a physician:
Do I feel unsteady?
Do I have the sensation that the room is spinning around me, even if just for a bit of a moment? Even if I’m seated or standing stationary, do I get the sensation of movement? Is it possible that I will lose my footing and fall? Do I get the feeling that I’m about to fall? Do I feel queasy or on the verge of passing out? Is there a problem with my vision? Is there ever a time when I feel puzzled, as if I’ve lost sense of time or location? What can I do to aid my physician in diagnosing me? You can help your doctor in diagnosing and creating a treatment plan by answering the following questions.
Prepare to share this information at your visit with your doctor. My dizziness or difficulty with my balance is best characterised as follows: Is there a sense of spinning, and if so, in which direction does it spin? Does a specific movement trigger the dizziness/twisting, or does it occur regardless of whether I sit or lie still? Are there any other symptoms associated with dizziness, such as hearing loss, tinnitus, a sensation of pressure in one or both ears, or headaches? Is there anything that can be done to alleviate the spinning and vertigo? How frequently do I get vertigo or loss of balance? How long do episodes of dizziness or spinning last (seconds, minutes, hours, or days)?
Is this my first fall? When did I lose my equilibrium? What became of me? What caused my fall? I’ve been knocked down an innumerable number of times. These are the medications I take. Include all prescription and OTC drugs, such as aspirin, antihistamines, and sleeping pills, as well as any vitamin supplements and alternative or homoeopathic remedies: Nomenclature du médicament or du complément. How much (milligrammes) and how frequently (times) do you take each day? This drug is being used to treat the following conditions. What types of research are being performed on vestibular diseases?
Scientists funded by the National Institute on Deafness and Other Communication Disorders (NIDCD) are studying animal ears to determine whether inner ear components that improve balance lost as a result of ageing, medications, infections, or trauma can be recovered in people with balance disorders. Other NIDCD-funded researchers are evaluating vestibular prosthesis, which are tiny devices that may be worn on the outside of the body or implanted in the ear to regulate the balance organs of the inner ear and alleviate dizziness.
Brought To You By; Ear Wax Removal Slough
First found On : https://forgottenportal.com/
The Article Autoimmune Inner Ear Disease – How Are Balance Disorders Treated First Appeared ON
: https://gqcentral.co.uk
The post Autoimmune Inner Ear Disease – How Are Balance Disorders Treated appeared first on https://alef3.com




Comments are closed